Exploring the Vagus Nerve: A Key Player in Sensory Processing Disorder
Share

Vagus nerve explained
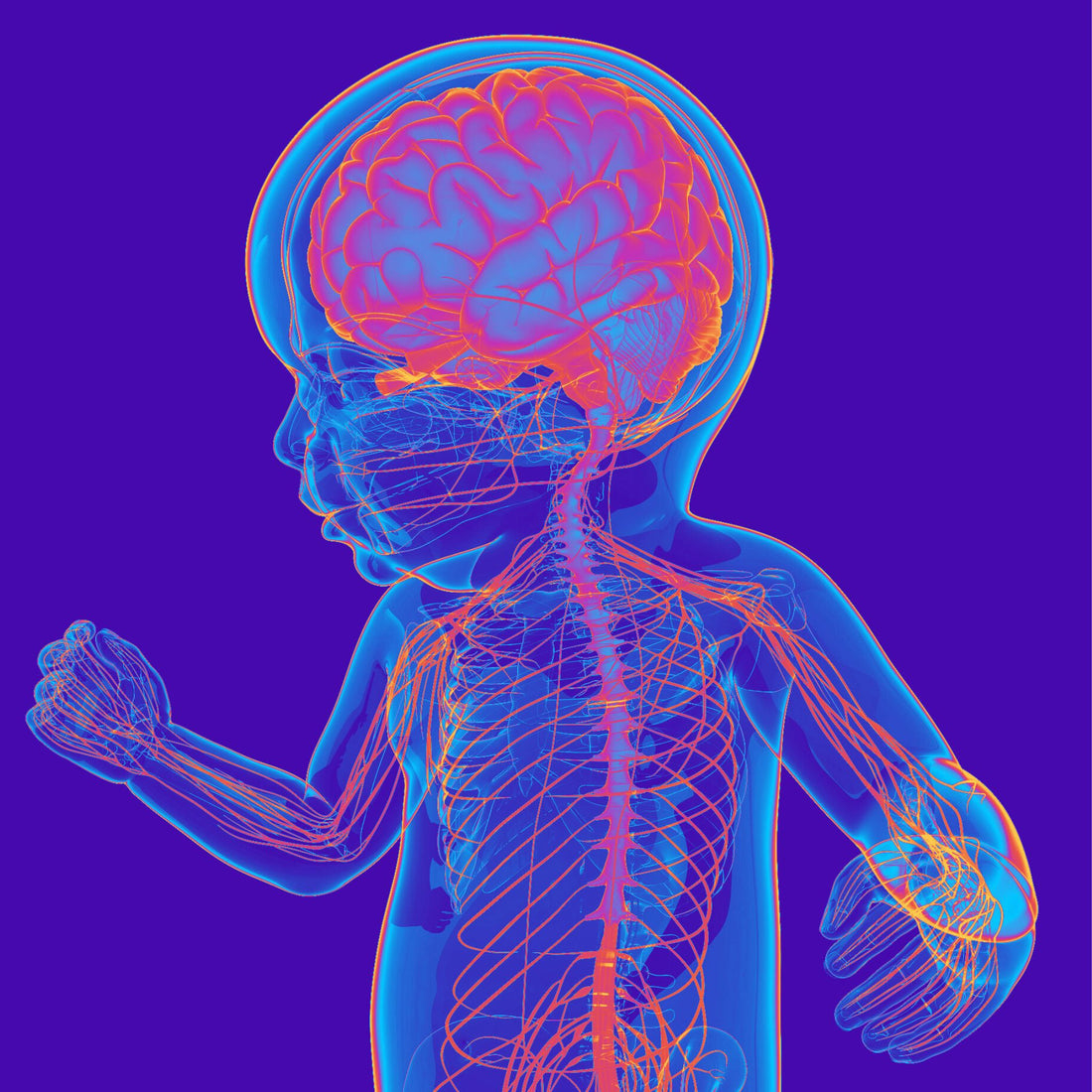
In the intricate network of the human nervous system, the vagus nerve stands out as a vital conductor of communication between the brain and the body. With its extensive reach and multifaceted functions, the vagus nerve plays a crucial role in regulating various bodily processes, including those related to sensory perception. In recent years, researchers have increasingly turned their attention to the vagus nerve's involvement in sensory processing disorders (SPD), shedding light on its profound impact on these conditions.
Sensory processing disorder is a condition in which the brain has difficulty receiving and responding to information that comes through the senses. Individuals with SPD may experience hypersensitivity or hyposensitivity to sensory stimuli, leading to challenges in regulating their responses to everyday sensations such as touch, sound, taste, and smell. While the precise causes of SPD remain under investigation, emerging evidence suggests that dysregulation of the vagus nerve may contribute significantly to its development and manifestation.
To understand the connection between the vagus nerve and sensory processing disorder, it's essential to grasp the role of this cranial nerve in the nervous system. The vagus nerve, also known as the tenth cranial nerve or CN X, is the longest and most complex of the cranial nerves, extending from the brainstem to multiple organs throughout the body. It serves as a crucial component of the autonomic nervous system, which controls involuntary bodily functions such as heart rate, digestion, and respiratory rate.
One of the vagus nerve's primary functions is to regulate the parasympathetic nervous system, often referred to as the "rest and digest" system. Through its extensive network of fibers, the vagus nerve influences various bodily organs, including the heart, lungs, digestive tract, and even the muscles involved in speech and swallowing. Importantly, the vagus nerve also plays a key role in modulating the body's response to stress and regulating emotional states, making it a central player in the body's overall state of balance and well-being.
In the context of sensory processing disorder, disruptions in vagal tone, which refers to the activity of the vagus nerve, have been implicated in the sensory dysregulation observed in affected individuals. Research suggests that individuals with SPD may exhibit alterations in vagal tone, leading to difficulties in effectively modulating sensory input and regulating emotional responses. For example, individuals with hypersensitivity to sensory stimuli may have heightened sympathetic arousal and decreased parasympathetic activity, contributing to their heightened reactivity to sensory input.

Furthermore, the vagus nerve's role in the gut-brain axis has garnered significant attention in recent years, with growing evidence linking gut health to neurological function and emotional regulation. The vagus nerve serves as a crucial conduit for bidirectional communication between the gut and the brain, allowing for the transmission of signals that influence mood, behavior, and cognitive function. Disruptions in this communication pathway, such as those seen in gastrointestinal issues or dysbiosis, may contribute to sensory processing difficulties and emotional dysregulation in individuals with SPD.
Moreover, interventions targeting vagal tone have shown promise in addressing sensory processing disorder symptoms and improving overall well-being in affected individuals. Techniques such as deep breathing exercises, mindfulness practices, and vagus nerve stimulation have been proposed as potential strategies to enhance vagal tone and promote sensory integration. By modulating the activity of the vagus nerve, these interventions aim to restore balance to the autonomic nervous system, thereby alleviating sensory sensitivities and improving emotional resilience.
In addition to its direct influence on sensory processing, the vagus nerve may also interact with other neural pathways implicated in SPD, including the oxytocin system and the endocannabinoid system. Oxytocin, often referred to as the "love hormone," plays a crucial role in social bonding, trust, and emotional regulation. Studies have shown that oxytocin levels and vagal tone are closely intertwined, with oxytocin release being facilitated by vagal activation. Dysregulation of the oxytocin system may contribute to difficulties in social interaction and emotional processing observed in individuals with SPD.
Similarly, the endocannabinoid system, which regulates neurotransmitter release and synaptic plasticity, has been implicated in sensory processing and emotional regulation. Endocannabinoid receptors are abundant in areas of the brain involved in sensory perception and emotional processing, suggesting a potential role in modulating sensory experiences and responses to stimuli. The vagus nerve interacts with the endocannabinoid system through its influence on gut health and inflammation, further highlighting its relevance to sensory processing disorder.
In conclusion, the vagus nerve emerges as a central player in the complex interplay between the nervous system, the gut, and emotional regulation, with profound implications for sensory processing disorder. Dysregulation of vagal tone and disruptions in vagal signaling pathways may contribute to the sensory sensitivities, emotional dysregulation, and social difficulties characteristic of SPD. By understanding the role of the vagus nerve in sensory processing, researchers and clinicians may uncover new avenues for intervention and support for individuals living with this challenging condition. Through targeted interventions aimed at enhancing vagal tone and restoring balance to the autonomic nervous system, individuals with SPD may find relief and improved quality of life.